Macular Degeneration
Age related macular degeneration (ARMD)
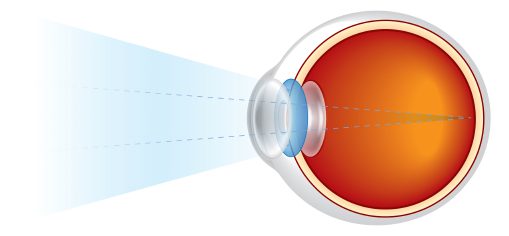
Age-related macular degeneration (ARMD) is a degenerative disease which affects a very small part of the retina at the back of your eye, called the macula. The macula gives us the clarity and fine detail of our central vision. Your central vision is the vision you use when you’re looking straight at something, for example when you’re reading, looking at photos or watching television.
In advanced forms of ARMD central vision can become distorted or blurry over a short period of time and a blank patch may appear in the centre of your vision. ARMD doesn’t affect your peripheral (side) vision, so it doesn’t cause total loss of sight.
Early ARMD often has no symptoms until the condition is more advanced and your vision is affected. As such, it is very important you have regular eye tests so ARMD can be caught early, and your vision preserved.
Symptoms can vary from person to person, but here are some of the symptoms associated with advanced stages of ARMD:
- Painless and constant blurring of central vision for far and near vision.
- Inability to see fine details like small text.
- Distortion or bending of straight lines.
- Visual hallucinations (seeing things that aren’t there).
- Objects looking smaller or larger than normal.
- Loss of ability to discern colours.
- Gaps or black spots in the central visual field.
- Slow recovery to dark after exposure to light and vice versa.
- Loss of contrast sensitivity.
- Problems with night driving.
.

Fig 1a- showing blood in macula area

Fig 1b- showing normal macula and retina
There are two types of Macular Degeneration: –
Dry macular degeneration is the most common form of the disease, somewhere between 85% and 90% of cases will be dry macular degeneration, which typically involves slow, gradual damage to the light-sensing cells in the retina. The dry form of macular degeneration involves the accumulation of small, yellowish lipid-deposits called drusen. These deposits can be present even in normal individuals, and likely do not cause age-related macular degeneration, but having drusen increases a person’s risk of developing macular degeneration.
Dry ARMD usually only causes mild loss of central vision but as the condition advances a small proportion of patients with dry ARMD can have significant loss of central vision. Although there is currently no treatment to restore vision lost from the advanced dry form of this disease, use of certain multivitamin supplements can slow down the progression of the condition. There are many studies currently underway to try to find an effective treatment.
Wet macular degeneration affects only about 10- 15% of people who have ARMD but it accounts for 90% of the people who have blindness from ARMD. The main problem is that wet ARMD results from age related wear and tear of a barrier (bruchs membrane) which keeps blood vessels in the choroid layer apart from the retina. Choroid is the most vascular part of the body, full of ‘leaky’ blood vessels to help oxygenation of retina. Retina by contrast has no leaky blood vessels under normal circumstances. As this barrier breaks down blood, ‘’leaky’’ blood vessels from the choroidal layer grow into the retina and start leaking blood and fluid in the macula area. Disorganisation of the macula photoreceptors results in visual failure and distortion.
For animation of wet AMD please see this link.
ARMD Management
The current management of those diagnosed with wet ARMD is through a series of injections into the jelly part of the eye under local anaesthetic. Lucentis, Avastin, Eylea and Beovu are all treatment choices that are available to you. This group of drugs are known as anti-vascular endothelial growth factor agents (anti VEGF). Eylea, Lucentis and Beovu are licensed products in UK and are available for treatment of wet ARMD as long as certain clinical criteria are met such as your level of vision at presentation and absence of scarring at the macula. These injections aim primarily to halt progression of abnormal blood vessels and stop the leaking and bleeding in the retina. These drugs prevent significant visual loss in 90% of cases (significant is defined as loss of more than 15 letters in ETDRS charts used in trials) and even improve vision (up to 30%-40%). You can expect that for the first 2 years you will be seen in on a regular basis (monthly) though depending on treatment pathway and response these appointments can be decreased in frequency.
Several risk-factors have been linked to macular degeneration such as increasing age, race and family history. Some other risk factors can be adjusted such as smoking, obesity and high blood pressure.
Individuals with advanced macular degeneration may have significant difficulty with normal tasks such as reading, paying bills, using a telephone, and other daily activities. In as much as the central vision may be severely diminished, options exist to try and help increase the projection of images from being focused on just the damaged area of the macula to being projected onto the areas of the retina that remain healthy and unaffected by the disease. This can be done via handheld magnifiers, digital magnification devices, phones with larger buttons, and various other features available on a smartphone or computer. In majority of cases the success of such interventions is limited. By far the best way to prevent vision loss from wet AMD is to catch the condition early and start treatment early.
What does the future hold for ARMD?
I lecture at Eastbourne Macular Disease Society on a yearly basis on this very subject.
You can contact Eastbourne macula society (Ellie – 07973508567) for information on lectures. Please come along and hear the most recent exciting research in this fascinating field.
Current research projects (list not exhaustive)
- Ways of preventing dry turning wet through injections
- Tablets and/or drops for preventing progression of dry ARMD
- Injecting agents to last longer for wet ARMD
- Radiotherapy for wet ARMD
- Reducing invasiveness in treatment of wet ARMD (tablets or drops)
- Stem cell therapy in ARMD
- Telescopic lens placement in advanced ARMD
What do I do if I think I have Macular Degeneration?
If you are concerned that you may have Macular Degeneration or would like more information do get in touch via the contact page.