Diabetic Retinopathy (DR)
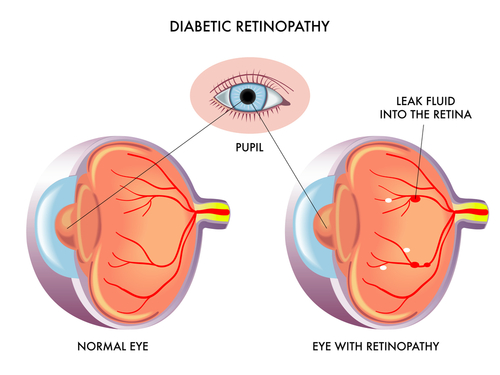
How can diabetes affect the eye?


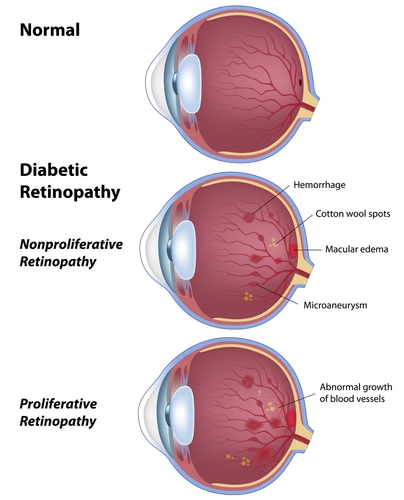
How do I know if I have diabetic eye disease?
What are the treatment options?
Intravitreal anti VEGF: Lucentis, Avastin and Eylea injections are the main pharamacotheraputic agents used to manage DMO. These drugs are injected in to the vitreous cavity. Lucentis and Eylea are approved for patients diagnosed with DMO on the NHS. However NICE has placed 400um of central oedema as a precondition for treatment. This is nearly twice the normal amount of macula thickness and undoubtedly there will be patients who will benefit from this treatment but sadly NHS will not provide cover for them. These patients may decide to have laser or IVTA (see below) if this is appropriate or fund the anti VEGF treatment themselves. Avastin (off label and off license) is a more cost effective alternative to lucentis and there is ample evidence for its effectiveness in patients with diabetic macular oedema. Both Lucentis and Avastin have a good chance of improving vision (up to 45%) unlike laser which tends to stabilize vision in general.
These injections are given monthly and usually are repeated to control the disease as the condition cannot be cured. The frequency of injections will vary between cases and will also depend on severity of the presenting condition. However the studies indicate that with time the need for injections is significantly reduced especially after the first year of treatment. Controlling your diabetes, hypertension and cholesterol are all vital in managing diabetic retinopathy. The treatments mentioned here should be used in adjunct in ensuring that your general medical conditions are also optimised.
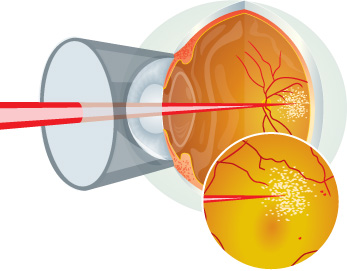
Laser: Macular laser was the first line of treatment for DMO (Fig D1) prior to arrival of anti VEGF injections and is the first choice if the retinal thickness is less than 400um, as this is a precondition for patients accessing anti VEGF on NHS. Macular laser helps to reduce macula fluid though it can cause damage to the retinal tissue. Macular laser may also not be possible if DMO involves the very centre of macula.. Laser mainly stabilizes vision by preventing further vision decline. It often will not improve vision. We have seen decline in use of macula laser since advent of anti VEGF injections.
Intravitreal Triamcelenone (IVTA): injection of unpurified steroid in to the globe could be an option if the patient has laser resistant DMO and is losing vision. IVTA is off license and off label and carries many side effects including cataract formation and raised eye pressure sometimes even causing glaucoma. These side effects could offset any potential gain from its use though the advantage of this mode of therapy is it can be offered through the NHS and may be of potential value in those who have had cataract surgery.
What should I expect after an injection?
Take home message is if in doubt please call in and get your symptom checked.
What are the risks with injection treatment?
Major risks (uncommon)
Serious eye infection (1 in every 1000 injections)
- Very high pressure in the eye
- Tear or detachment in the retina
- Traumatic cataract
- Blood clots or bleeding inside the eye
- Inflammation in the eye
- Potential for heart attack and/or stroke – only theoretical
Minor risks (common)
- Red eye (bleed at the superficial surface of the eye)
- Sore gritty eye (usually first 48 hours post injection)
- Small specks (floaters ) or transient flashing lights may be seen in your vision for few days
What is the difference between anti VEGF injection like Lucentis and an Ozurdex implant?
Can I have cataract surgery if I have diabetic eye disease?
What are the advantages of private treatment?
Most insurance companies, if you are insured will fund the treatment to a certain point depending on your level of cover and thankfully in most cases we can treat sub 400um if treatment is deemed beneficial by the clinician.
NICE website guidance link
Ranibizumab for treating diabetic macular Odema
Dexamethasone intravitreal implant for treating diabetic macular oedema
Aflibercept for treating diabetic macular oedema
https://www.nice.org.uk/guidance/ta346?unlid=60414705620161623933
For more information on Retinal disorders please read the below pages: